Uncovering the Essential Relationship Between Mental Health and Gut Health in the UK
Exploring the Complex Mechanisms of the Gut-Brain Axis
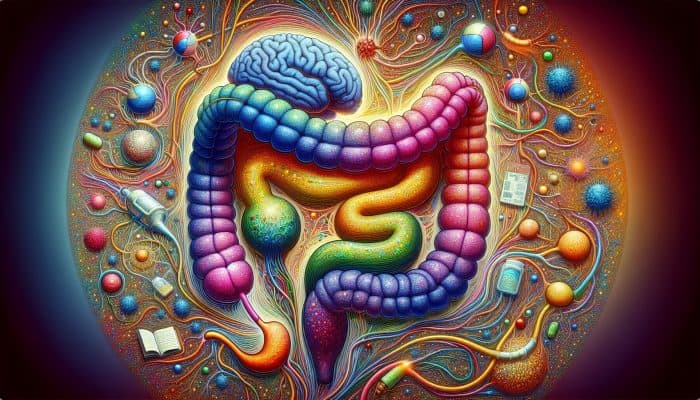
The gut-brain axis represents a sophisticated communication network that connects the gastrointestinal system with the central nervous system, playing a crucial role in both mental health and emotional wellness. This intricate system operates through a myriad of neural, hormonal, and immunological signals, enabling continuous feedback between the gut and the brain. The gut, often termed the “second brain,” contains a vast array of neurons and has a unique capability to synthesize neurotransmitters such as serotonin, predominantly found in the digestive tract. Recognizing the profound impact of gut health on mental health and emotional stability is essential for effective wellness strategies, as it opens avenues for holistic interventions that prioritize both physical and emotional well-being.
Recent studies indicate that our gut microbiome—the rich ecosystem of microorganisms residing within our intestines—significantly influences our mood and overall mental health. An imbalance in gut bacteria, known as dysbiosis, has been connected to various mental health disorders, including anxiety and depression. This correlation is particularly important in the UK, where factors like economic pressures and social isolation tend to worsen mental health challenges. Understanding the mechanisms of this gut-brain communication is vital for creating more holistic approaches to mental health treatment, incorporating dietary adjustments and lifestyle enhancements to foster better gut health, enhancing emotional resilience, and improving overall quality of life.
Examining the Rising Incidence of Mental Health Disorders in the UK
Mental health disorders are alarmingly prevalent in the UK, affecting millions of individuals annually. Recent statistics show that approximately one in four adults will face a mental health issue each year, with anxiety and depression emerging as the most common disorders. These challenges not only disrupt individual lives but also place immense strain on the healthcare system, leading to a heightened demand for mental health services. The COVID-19 pandemic has exacerbated these issues, with rising reports of anxiety and loneliness becoming widespread, further emphasizing the urgency for innovative and comprehensive treatment solutions.
The high prevalence of mental health disorders highlights an urgent call for innovative treatment options, particularly those that consider the integral role of gut health. Ongoing research is uncovering the connection between gut microbiota and mental wellness, leading to increased awareness of how dietary changes and interventions focusing on gut health can function as effective complementary therapies for managing mental health conditions. By prioritizing gut health, we may uncover new pathways to enhance mental well-being and resilience against psychological distress.
Understanding the Impact of Diet on Mental Well-Being
Diet significantly influences mental health, with emerging research suggesting that our food choices can directly affect mood and cognitive performance. In the UK, traditional diets often high in processed foods, sugars, and unhealthy fats may contribute to negative mental health outcomes. Conversely, diets abundant in whole foods—especially those rich in fiber, vitamins, and healthy fats—can promote a thriving gut microbiome and, in turn, enhance mental wellness. The foods we consume play a pivotal role in shaping our emotional landscape, requiring increased awareness of dietary patterns and their implications for mental health.
Certain nutrients are particularly important for brain health, including omega-3 fatty acids, B vitamins, and antioxidants. For instance, omega-3 fatty acids, predominantly sourced from oily fish like salmon, can help mitigate inflammation and stimulate neurogenesis, which is vital for maintaining cognitive function. Additionally, B vitamins are essential for the synthesis of neurotransmitters, influencing mood regulation and emotional stability. A diet rich in fruits, vegetables, and whole grains supports a healthy gut microbiome, increasingly recognized as a key foundation for good mental health. Making conscious dietary choices can significantly bolster mental well-being and enhance resilience against mental health disorders, promoting a holistic approach to emotional health.
Expert Opinions on the Interconnection Between Mental Health and Gut Health

Real-Life Examples of How Gut Health Influences Mental Wellness
A wealth of anecdotal evidence from individuals throughout the UK underscores the significant effects of gut health on mental wellness. For example, a young professional from London recounted her transformative journey after adopting a gut-friendly diet. After years of battling anxiety and depression, she made a deliberate effort to improve her gut health by incorporating more fermented foods such as kefir and sauerkraut into her diet. Within a matter of weeks, she noticed a substantial decrease in her anxiety levels and an uplift in her overall mood, highlighting the powerful benefits of dietary changes and the potential for improved mental health through gut health optimization.
Similarly, a family from Manchester found that by eliminating processed sugars and embracing whole food options, their teenage son experienced a marked reduction in depressive episodes. These real-life cases emphasize the importance of prioritizing gut health as a viable strategy for managing mental health challenges. By sharing these experiences, we can inspire others to consider the profound impact that dietary and lifestyle changes can have on their mental health.
The key benefits of improving gut health include:
- Enhanced mood and emotional resilience
- Decreased symptoms of anxiety and depression
- Improved cognitive function and concentration
- Increased energy levels and reduced fatigue
- Better sleep quality
- Enhanced digestive health
- Overall improved quality of life
- Boosted self-esteem and motivation
Examining the Latest Findings in Gut Health and Mental Well-Being
Recent studies conducted in the UK have shed light on the complex relationship between gut microbiota and mental health, underscoring the necessity of maintaining a healthy gut for emotional stability. Research has identified particular strains of probiotics, including Lactobacillus and Bifidobacterium, that demonstrate positive effects on mood and levels of anxiety. These findings suggest that targeted probiotic supplementation could serve as a promising complementary therapy for those struggling with mental health disorders. By harnessing the power of these beneficial microorganisms, we may enhance mental health outcomes for a variety of individuals.
Key insights from these studies highlight that:
– Diversity of the gut microbiome correlates with improved mental health outcomes, indicating that a varied diet rich in different food sources can strengthen gut health.
– Certain dietary patterns, particularly those rich in fermented foods, support a healthy gut microbiome and thus contribute to better mental health.
– Prebiotics can amplify the effectiveness of probiotics by providing essential nourishment to beneficial gut bacteria, further enhancing mental health. Individualized treatment strategies targeting the gut-brain axis show promise for future mental health interventions, allowing for tailored approaches that cater to individual needs.
As researchers continue to explore this vital connection, it becomes increasingly evident that prioritizing gut health should be a fundamental aspect of mental health treatment approaches, paving the way for innovative and effective therapeutic options.
Implementing Practical Steps to Improve Gut Health

Improving gut health can be a manageable and straightforward task, with various dietary changes and lifestyle habits that individuals in the UK can adopt to boost their mental wellness. Here are some actionable suggestions:
1. Incorporate fermented foods: Integrating foods like yoghurt, kefir, kombucha, and sauerkraut can enhance gut microbiota diversity and promote a healthier digestive environment.
2. Increase fiber intake: Adding more fruits, vegetables, whole grains, and legumes provides prebiotics that nourish beneficial gut bacteria, supporting gut health and overall wellness.
3. Stay hydrated: Consuming adequate water supports digestion and overall gut health, contributing to better nutrient absorption and elimination.
4. Limit processed foods: Reducing sugar and unhealthy fats can help maintain a balanced gut microbiome, preventing dysbiosis and its associated mental health implications.
5. Consider probiotics: Supplementing with probiotics can help restore gut flora, particularly after antibiotic use, aiding in the recovery of gut health.
6. Engage in regular physical activity: Exercise enhances gut motility and can promote a healthier microbiome, contributing to both physical and mental well-being.
7. Effectively manage stress: Practices such as mindfulness, meditation, and yoga can positively affect gut health and emotional resilience.
Prioritize sleep: Ensuring sufficient and quality sleep is critical for maintaining both gut and mental health, allowing for restorative processes to occur.
Implementing these strategies can lead to significant enhancements in gut health, thereby improving mental well-being. By taking proactive steps, individuals can foster a healthier lifestyle that benefits both their gut and mental health.
Assessing the UK Healthcare System’s Response to the Gut-Mental Health Connection
Evaluating the Accessibility of Mental Health Services Across the UK
The National Health Service (NHS) in the UK offers a broad spectrum of mental health services, encompassing therapy, medication, and crisis intervention. However, accessing these services can often be difficult, with waiting times varying significantly by region. Urban areas may have more resources available but also face heightened demand, leading to longer wait times for treatment, which can be frustrating for individuals seeking timely support.
Successfully navigating the mental health services provided by the NHS necessitates a proactive approach. Individuals should seek referrals from their General Practitioner (GP) for any mental health concerns. GPs can then guide patients to appropriate resources, such as the Improving Access to Psychological Therapies (IAPT) program, which offers talking therapies targeting anxiety and depression, providing essential support to those in need.
It is essential for individuals to advocate for their health by actively engaging with their healthcare providers, exploring available options, and understanding their rights to timely access to care. Familiarity with local mental health resources empowers individuals to seek the support they require, facilitating a collaborative approach to wellness.
Integrating Gut Health into Mental Health Care Models
In recent years, there has been a growing recognition within the UK healthcare system about the importance of gut health in treating mental health disorders. Some forward-thinking healthcare providers have started to incorporate gut health assessments into mental health care plans. This comprehensive approach is gradually gaining traction, acknowledging the interconnectedness of physical and mental health and the importance of a holistic perspective.
Initiatives to weave gut health into mental health care include collaborations among dietitians, psychologists, and general practitioners, aimed at designing holistic care plans that address both gut and mental health needs. Moreover, training healthcare professionals to identify signs of gut-related health issues in patients presenting with mental health challenges is critical for early intervention and comprehensive treatment. This transition towards an integrated model of care seeks to deliver more effective and personalized mental health treatment, ensuring that all aspects of health are considered in the healing process.
Exploring the Role of Private Healthcare in Advancing Mental and Gut Health
Private healthcare options in the UK provide additional resources for those seeking specialized care concerning both mental and gut health. Numerous private clinics offer tailored services, which may include advanced nutritional assessments, gut microbiome analysis, and individualized dietary planning. These services can be particularly beneficial for individuals who have not found success with conventional methods or who desire a more comprehensive approach to their health and wellness.
However, opting for private care can also present challenges. Costs can be high, and not all services may be covered by health insurance. Additionally, the quality of care can vary significantly between providers, making it essential for individuals to thoroughly research potential private healthcare options and seek recommendations from trusted sources. Balancing the benefits against potential drawbacks will help individuals make informed decisions regarding their healthcare choices, ensuring they receive the best possible support for their needs.
Identifying Common Gut Health Issues in the UK and Their Psychological Impact
Examining the Prevalence of Irritable Bowel Syndrome (IBS) in the UK
Irritable Bowel Syndrome (IBS) is a prevalent condition in the UK, affecting around 20% of the population. This functional gastrointestinal disorder is characterized by symptoms such as abdominal pain, bloating, and altered bowel habits. Notably, IBS frequently correlates with mental health disorders, particularly anxiety and depression, creating a challenging cycle that can be difficult to break and debilitating for those affected.
The interplay between IBS and mental health is complex. Stress and anxiety can exacerbate IBS symptoms, while the discomfort and unpredictability of IBS can contribute to heightened feelings of anxiety and depression, creating a vicious cycle. It is essential for individuals suffering from IBS to pursue comprehensive treatment that addresses both gastrointestinal symptoms and mental health concerns. This may involve dietary modifications, psychological therapies, and stress management strategies, all aimed at enhancing overall quality of life and breaking the cycle of distress.
Understanding the Psychological Effects of Inflammatory Bowel Disease (IBD)
Inflammatory Bowel Disease (IBD), which includes Crohn’s disease and ulcerative colitis, can impose significant psychological challenges for those affected. The chronic nature of IBD, characterized by cycles of flare-ups and remission, often creates feelings of uncertainty and stress. Living with chronic pain and disruptions to daily life can lead to the development of anxiety and depression in individuals with IBD, impacting their overall quality of life.
The psychological implications of living with IBD may encompass increased feelings of isolation, frustration, and helplessness. Thus, healthcare providers must adopt a multidisciplinary approach to managing IBD, addressing not only physical symptoms but also providing psychological support. Cognitive Behavioral Therapy (CBT) and support groups can serve as effective resources for individuals grappling with the mental health implications of IBD, fostering resilience and coping strategies that empower individuals to navigate their challenges.
Exploring the Psychological Impact of Celiac Disease
Living with celiac disease necessitates strict adherence to a gluten-free diet, which can introduce various social and psychological challenges. The rigorous dietary management required for celiac disease often leads to feelings of social isolation, especially in social settings involving food. The anxiety surrounding potential gluten exposure can amplify stress levels and have adverse effects on mental health, necessitating additional support for individuals navigating these challenges.
Individuals with celiac disease can protect their mental well-being by participating in support groups that focus on celiac disease, fostering community and shared understanding. Furthermore, education about navigating a gluten-free lifestyle empowers those affected, equipping them with essential tools to manage social situations with confidence. Mental health professionals should also be aware of the psychological effects associated with celiac disease and offer strategies to mitigate anxiety and promote a positive outlook, ensuring a holistic approach to care.
Assessing the Mental Health Effects of Gastroesophageal Reflux Disease (GERD)
Gastroesophageal Reflux Disease (GERD) is another gastrointestinal condition that can considerably impact mental health. The discomfort associated with GERD, including heartburn and sleep disturbances, can elevate stress and anxiety levels. The chronic nature of GERD may leave individuals feeling fatigued and overwhelmed, further intensifying mental health concerns and disrupting daily life.
Effectively managing GERD often requires lifestyle changes such as dietary adjustments, weight management, and stress reduction techniques. By addressing GERD symptoms, individuals may also experience improvements in their mental health, as alleviating physical discomfort can lead to reduced stress and anxiety. Comprehensive treatment plans should encompass both physical and mental health considerations to ensure a holistic approach to care that promotes overall well-being.
Understanding the Connection Between Gut Infections and Mood Disorders
Gut infections can disrupt the delicate balance of the gut microbiome, contributing to mood disorders such as depression and anxiety. Pathogen-induced infections can trigger inflammation and dysbiosis, affecting neurotransmitter production and gut-brain communication. Understanding the mental health consequences of chronic gut infections is essential for effective treatment and recovery.
Individuals experiencing gut infections should promptly seek medical attention to address the underlying causes of their symptoms. Treatment may involve antibiotics or probiotics to restore gut balance. Additionally, mental health support should be considered, as individuals may experience anxiety related to their health conditions. Strategies such as mindfulness practices, cognitive-behavioral therapies, and emerging therapies may offer tools for managing the psychological impact of chronic gut infections, fostering resilience and emotional stability.
Exploring Dietary Patterns in the UK and Their Impact on Mental Health
Investigating the Traditional British Diet and Its Effects on Mental Wellness
The traditional British diet, often characterized by high consumption of processed foods, sugars, and unhealthy fats, can be detrimental to mental health. Many typical British meals lack the essential nutrients required for a healthy gut microbiome, which in turn can affect mood, cognitive function, and overall mental well-being. The prevalence of convenience foods and takeaways exacerbates these dietary challenges, perpetuating a cycle of poor nutritional choices and declining mental health.
To combat these trends, individuals can explore healthier alternatives within the framework of UK dietary culture. Prioritizing whole foods, such as fruits, vegetables, lean proteins, and whole grains, can significantly enhance mental health outcomes. Additionally, incorporating traditional British foods like porridge, roasted vegetables, and fish can provide nutrient-dense options that positively contribute to mental wellness, promoting a balanced approach to nutrition.
The Benefits of Adopting a Mediterranean Diet for Mental Health
Embracing a Mediterranean diet, which is rich in fruits, vegetables, whole grains, and healthy fats like olive oil, has been associated with improved mental health outcomes. This dietary pattern correlates with lower levels of depression and anxiety, likely due to its anti-inflammatory properties and beneficial effects on gut health. The Mediterranean diet encourages the intake of nutrient-dense foods that promote a diverse and thriving gut microbiome, thus supporting emotional wellness.
Residents in the UK can incorporate principles of the Mediterranean diet into their daily lives by including more plant-based meals, utilizing olive oil for cooking, and opting for fresh produce. Sharing meals, a vital aspect of Mediterranean culture, can also enhance social connections and emotional wellness. Simple dietary swaps, such as replacing white bread with whole-grain alternatives or enjoying a vegetable-rich salad, can lead to noticeable improvements in mental health outcomes, highlighting the importance of diet in emotional well-being.
The Advantages of a Plant-Based Diet for Enhancing Mental Health
A plant-based diet has been linked to enhanced gut health and reduced inflammation, both of which can positively influence mental health. This dietary approach emphasizes the consumption of fruits, vegetables, legumes, nuts, and whole grains, which are abundant in fiber, vitamins, and antioxidants. Research indicates that individuals adhering to a plant-based diet often report lower rates of anxiety and depression compared to those following more traditional dietary patterns, reinforcing the connection between diet and mental wellness.
Key plant-based foods that support mental health include:
- Leafy greens (e.g., spinach, kale)
- Berries (e.g., blueberries, strawberries)
- Walnuts and flaxseeds (rich in omega-3 fatty acids)
- Legumes (e.g., lentils, chickpeas)
- Whole grains (e.g., brown rice, quinoa)
- Fermented foods (e.g., kimchi, sauerkraut)
- Avocado (healthy fats)
- Sweet potatoes (rich in vitamins and minerals)
Incorporating these specific foods into daily meals can enhance gut health, potentially leading to improvements in mental health and overall well-being. By focusing on nutrient-dense foods, individuals can cultivate a diet that supports both their physical and mental health.
Research-Backed Benefits of the Interconnection Between Mental Health and Gut Health
Insights from Experts on the Role of Probiotics in Mental Wellness
Probiotics have a significant impact on mental health by modifying the gut microbiota. Certain strains of probiotics have been shown to offer psychological benefits, with research indicating that Lactobacillus and Bifidobacterium species can effectively alleviate symptoms of anxiety and depression. These probiotics facilitate communication within the gut-brain axis, promoting the synthesis of neurotransmitters such as serotonin and gamma-aminobutyric acid (GABA), both critical for mood regulation and emotional balance.
Incorporating probiotic-rich foods, such as yoghurt and other fermented products, into the diet can be an effective strategy for improving mental health. Additionally, targeted probiotic supplementation tailored to individual needs can optimize these benefits, potentially leading to meaningful improvements in emotional well-being. As research continues to evolve, understanding which specific strains provide the most psychological advantages will be essential for developing effective interventions focused on mental well-being.
The Contribution of Prebiotics to Mental Health Enhancement
Prebiotics serve as nourishment for beneficial gut bacteria, promoting their growth and activity. By enhancing the gut microbiome, prebiotics may lead to improved mental health outcomes. The best sources of prebiotics within the UK diet include foods like garlic, onions, leeks, asparagus, bananas, and oats. These foods not only support gut bacteria but also contribute positively to overall digestive health, creating a foundation for mental wellness.
Research suggests that the consumption of prebiotics can elevate mood and reduce anxiety levels, highlighting their potential role in bolstering mental health. As individuals strive to enhance their mental well-being, increasing the intake of prebiotic-rich foods can serve as a simple yet effective strategy for supporting both gut and mental health, emphasizing the importance of nutrition in overall wellness.
Long-Term Benefits of Prioritizing Gut Health
Long-term research indicates that maintaining robust gut health can lead to sustained improvements in mental health. Individuals who actively engage in gut health interventions, including dietary changes and regular physical activity, frequently report better mental health outcomes over time. These interventions can help cultivate a balanced gut microbiome, reduce inflammation, and optimize neurotransmitter production—all crucial factors for mental wellness.
Key findings from these long-term studies include:
– Individuals with a healthy gut microbiome experience lower rates of mood disorders, demonstrating the importance of gut health in emotional regulation.
– Dietary strategies that support gut health yield lasting positive impacts on mental health, underscoring the connection between nutrition and psychological well-being.
– Regular monitoring and adaptation of gut health strategies can lead to sustained improvements in overall well-being, encouraging individuals to prioritize their gut health as a pathway to enhanced mental wellness.
By prioritizing gut health, individuals can achieve not only temporary relief from mental health challenges but also lasting enhancements in their quality of life, reinforcing the vital link between physical and mental health.
Strategies for Enhancing Gut Health for Improved Mental Wellness in the UK
The Significance of Regular Exercise for Gut and Mental Health
Regular physical activity is essential for improving gut health and alleviating symptoms of mental health disorders. Engaging in exercise stimulates gut motility, enhances blood flow to the digestive system, and encourages the growth of beneficial gut bacteria. Moreover, physical activity releases endorphins and increases serotonin levels, contributing to improved mood and reduced anxiety, creating a positive feedback loop for mental wellness.
Types of exercise particularly beneficial for gut and mental health include aerobic activities such as walking, jogging, cycling, and swimming, as well as strength training and mind-body exercises like yoga and tai chi. Individuals should aim for at least 150 minutes of moderate-intensity exercise weekly, mixing various activities to maintain an enjoyable routine. By prioritizing regular exercise, residents of the UK can effectively enhance both their gut health and mental well-being, promoting a lifestyle that supports physical and emotional resilience.
Integrating Effective Stress Management Techniques
Stress adversely affects both gut health and mental well-being, creating a cycle of worsening symptoms that can be challenging to break. Adopting effective stress management techniques can help alleviate these effects and improve overall wellness. Strategies that individuals in the UK can implement include mindfulness meditation, deep breathing exercises, progressive muscle relaxation, and engaging in hobbies that promote relaxation and enjoyment, fostering a sense of peace and balance.
Additionally, spending time in nature, practicing gratitude, and nurturing connections with friends and family can further enhance stress management efforts. By integrating these strategies into their daily lives, individuals can cultivate resilience against stress, thereby boosting both gut health and mental wellness, highlighting the importance of emotional support in overall health.
Recognizing the Essential Role of Sleep in Supporting Gut and Mental Health
Quality sleep is critical for maintaining both gut health and mental well-being. Poor sleep can disrupt the balance of gut microbiota and negatively affect neurotransmitter production, leading to heightened anxiety and depressive symptoms. Conversely, a healthy gut can contribute to better sleep quality, establishing a reciprocal relationship between these two vital health aspects that underscores the importance of holistic health practices.
Residents in the UK can enhance their sleep quality by establishing a consistent sleep schedule, creating a calming bedtime routine, optimizing their sleep environment, minimizing caffeine and screen time before bed, and practicing relaxation techniques, all of which can improve sleep hygiene and overall health. Prioritizing sleep can significantly enhance an individual’s gut health and support their mental wellness, emphasizing the interconnectedness of physical and mental well-being.
Utilizing Supplements to Enhance Mental and Gut Health in the UK
Identifying the Most Beneficial Supplements for Gut Health
Several supplements can effectively support gut health, potentially leading to improved mental health outcomes. For UK residents, omega-3 fatty acids and vitamin D are particularly noteworthy. Omega-3s, found in fish oil and algal oil supplements, possess anti-inflammatory properties that benefit both gut and mental health. Meanwhile, vitamin D is essential for immune function and has been linked to mood regulation, highlighting the importance of adequate nutrient intake for emotional wellness.
Other beneficial supplements include magnesium, which supports relaxation and improves sleep quality, as well as prebiotic fibers that nourish gut bacteria. Before starting any supplementation routine, individuals should consult with a healthcare professional to determine the appropriate dosage and ensure safety, particularly concerning existing health conditions or medications. By taking a thoughtful approach to supplementation, individuals can enhance their overall health and well-being.
Evaluating the Mental Health Benefits of Probiotic Supplements
Probiotic supplements have gained popularity for their potential to alter gut microbiota and enhance mental health. Research indicates that specific strains, such as Lactobacillus rhamnosus and Bifidobacterium longum, may be particularly effective in alleviating symptoms of anxiety and depression. The effectiveness of these supplements can vary based on the strain used and the individual’s unique microbiome, necessitating personalized approaches to supplementation.
When selecting probiotic supplements, individuals should consider factors such as the number of colony-forming units (CFUs), the diversity of strains, and expiration dates. It is also critical to integrate probiotics into a balanced diet that supports overall gut health to maximize their potential benefits for mental wellness, ensuring a comprehensive approach to health.
Understanding the Risks and Benefits Associated with Supplements
While supplements can offer significant advantages, they also carry potential risks and interactions that UK residents should remain aware of. Relying excessively on supplements without addressing dietary and lifestyle factors can create nutrient intake imbalances. Additionally, certain supplements may interact with medications, leading to adverse effects that necessitate careful consideration.
Individuals should approach supplementation with caution, prioritizing a balanced diet and consulting healthcare providers for guidance. Monitoring for any side effects and adjusting dosages as necessary can help mitigate risks while maximizing the benefits of supplements for gut and mental health, fostering a holistic approach to health management.
Future Directions for Research on the Interconnection of Mental Health and Gut Health in the UK
Exploring Innovative Therapies and Interventions
Current research in the UK is delving into pioneering therapies, including faecal microbiota transplantation (FMT), which shows promise in enhancing both gut and mental health. FMT involves transferring microbiota from a healthy donor to a recipient, potentially restoring a balanced gut microbiome. Preliminary studies suggest that FMT may offer benefits for certain mental health conditions, although extensive research is necessary to validate these findings and understand the long-term implications.
As our understanding of the gut-brain axis deepens, new therapeutic approaches integrating gut health into mental health treatment are likely to emerge. This could yield personalized interventions tailored to individual microbiome profiles, thereby providing more effective mental health care that acknowledges the complexity of human health.
Leveraging Technology for Monitoring Gut Health
The increasing prevalence of wearable technology and mobile applications presents exciting opportunities for monitoring gut health and supporting mental health management. Various apps enable users to track dietary intake, symptoms, and mood fluctuations, fostering greater awareness of the connections between gut health and mental well-being.
Residents in the UK can leverage these technologies to identify patterns and correlations, empowering them to make informed choices regarding their dietary and lifestyle habits. Furthermore, wearable devices can monitor physical activity and stress levels, offering valuable insights into overall health. As technology continues to advance, it will play an essential role in facilitating personalized health management strategies that enhance both gut and mental health.
Identifying Research Priorities for Future Exploration
Future research in the UK should concentrate on developing personalized approaches to gut and mental health, taking into account individual dietary and lifestyle variables. This may involve large-scale studies examining the effects of specific dietary patterns on gut health and mental well-being across diverse populations, providing insights that can inform public health strategies.
Moreover, investigating the role of the gut microbiome in mental health disorders beyond anxiety and depression—including conditions such as schizophrenia and bipolar disorder—represents a promising area for further exploration. Research should also evaluate the long-term impacts of dietary interventions on mental health outcomes, contributing to the creation of evidence-based guidelines for enhancing mental wellness through improved gut health.
Integrating Gut and Mental Health Services in the UK
Efforts are underway to integrate gut and mental health services within the UK, with the goal of providing holistic care that concurrently addresses both aspects. This integration could involve collaboration among gastroenterologists, psychiatrists, dietitians, and psychologists to develop comprehensive treatment plans for individuals facing challenges related to both gut and mental health, ensuring that all aspects of health are considered.
By fostering communication between these disciplines, healthcare providers can offer more effective personalized care, ultimately improving patient outcomes. As this integrated model continues to develop, it will pave the way for a more comprehensive understanding of health that encompasses the well-being of both the gut and the mind, promoting a holistic approach to health management.
Addressing Common Questions About Mental Health and Gut Health
What is the gut-brain axis?
The gut-brain axis is a bidirectional communication network linking the gastrointestinal tract with the central nervous system, influencing mental health and emotional well-being through neural, hormonal, and immunological signals. Understanding this connection is crucial for developing effective treatment strategies.
How does diet affect mental health?
Diet plays a critical role in mental health, with certain foods affecting mood and cognitive function. Nutrient-rich diets can promote gut health, which in turn can lead to improved mental well-being, emphasizing the importance of dietary choices.
Can probiotics improve mental health?
Yes, probiotics can positively influence mental health by promoting a healthy gut microbiome. Specific strains have been shown to alleviate symptoms of anxiety and depression, highlighting their potential as complementary therapies.
What are common gut health issues in the UK?
Common gut health issues in the UK include Irritable Bowel Syndrome (IBS), Inflammatory Bowel Disease (IBD), and Gastroesophageal Reflux Disease (GERD), all of which can impact mental health and emotional well-being.
What role does exercise play in gut health?
Regular exercise enhances gut motility, supports a healthy microbiome, and releases endorphins, all of which contribute to improved mental health and emotional stability.
How can I improve my gut health?
Improving gut health can be achieved through dietary changes, including increasing fiber intake, incorporating fermented foods, staying hydrated, and effectively managing stress, fostering a supportive environment for gut health.
What are the benefits of a plant-based diet?
A plant-based diet can enhance gut health and reduce inflammation, potentially leading to improvements in mental health, as nutrient-dense foods support both aspects of well-being.
What supplements can support gut health?
Supplements such as omega-3 fatty acids, vitamin D, and prebiotics can support gut health, potentially leading to improved mental health outcomes and overall wellness.
How does sleep affect gut and mental health?
Adequate sleep is crucial for maintaining gut health, as insufficient sleep can disrupt the gut microbiota and negatively impact mental well-being, highlighting the importance of quality rest.
What is the future of mental health and gut health research?
Future research should prioritize personalized approaches to gut and mental health, exploring the microbiome’s role in various mental health disorders and integrating treatment services for comprehensive care.
Connect with us on Facebook!
The Article Mental Health and Gut Health: A UK Perspective Was First Published On https://acupuncture-frome.co.uk
The Article Gut Health and Mental Wellbeing: Insights from the UK Was Found On https://limitsofstrategy.com
Leave a Reply